We need to develop immune resilience in order to survive this Covid-19 pandemic and any future pandemics. Here’s how the gut microbiome is intimately associated with the immune system. And how to nourish and nurture your microbiome.
Immune structures are located all over the body (in all mucosal linings and lymph nodes) and there is a two layered response to an invader.
The immediate response – is with the innate immune system. These cells (macrophages and dendritic cells) quickly tackle the invader with everything they have. Their response is a general response against any invader, whether it is a virus, bacteria, etc.
Think about what can happen if you have an infestation of ants into your house. The innate response would be like taking a poisonous pest spray and spray the ants and the house with it – you would kill not only the ants but any other insect and you would be creating an unhealthy environment in the house by using the pesticide.
The human innate response creates inflammation in the body. Sometimes that is the best and appropriate way to deal with the invasion or injury.
However, the response can be exaggerated and there can be collateral damage to tissues and cells. Sort of like the example above.
After a while, the second immune response kicks in, the adaptive immune system. These cells are like specialists – they each can target a specific type of invader with specialized equipment. However, they wait for signals from the innate responders and this can take some time.
Once they get there, the adaptive responders signal the first group to tone down the response and they will take over with a more elegant and specific approach to dealing with the invaders.
In the case of Covid, it appears that in some people, the first responders are not being signaled to stop the general overwhelming response.
We know that people with co-morbidities like diabetes, heart disease and other inflammatory conditions have a higher risk of having their innate response linger and never go into the adaptive response.
This is called a cytokine storm.
The inflammation created by the first responders is not resolved and leads to a vicious cycle of more inflammation and more tissue damage.
Why does this happen?
Immune cells are made in the bone marrow and thymus. They are sort of “born” as immature cells and they have to develop and mature in the local areas like lymph nodes and the peyers patches in the gut, before they are released into the circulation to do their job.
The signals for maturation – the “training” come from the microbiome. We see this in nobiotic mice – mice that have no bacteria in their gut. We see that the immune system is very poorly defined.
The energetics for responding to an immune infraction, comes from the microbiome. The microbiome produces the energy (butyrate) and the equipment for the immune system to work.
Inside the body everything is covered by a mucosa – to the order of 400 square meters, which translates to the flooring of a 4,000 foot house.
A pathogen enters the body through a mucosal layer such as the nose, mouth, eyes, urogentital tract or skin. The sampling and identification of a pathogen all takes place in the mucosal layer. The mucosa houses 40 trillion microbes.
How does the immune system sift through these trillions to find the few pathogens that can cause problems? There are about 200 million immune cells that can do that job. So it is 200 million immune cells to 40 trillion microbes – a 200,000 to one ratio – how does it actually do this successfully?
The only way to do this is if the other trillions can watch out for the immune system and when they sense a new pathogen entering the system the resident microbiota signals the immune system to come and take a look, sort of like a neighborhood watch. (This concept has been suggested by Kiran Krishnan in various interviews).
The mucosal layer of the gut is the largest sampling tissue in the body, because the gut is the largest site for the entrance of foreign material to the body. The mucosa is where everything that comes in through the mouth is inspected to see if it is friend or foe.
This is where oral tolerance is developed.
These sampling tissues learn what you are exposed to (both acutely and chronically) and then learn whether or not to attack them. For instance, the foods that you eat every day should not be attacked by the immune system. If they do, then it can lead to immune intolerance of those foods, which can cause symptoms and even serious anaphylactic responses to certain classes of food.
Food contain nutrients , but it also contains toxins and microbes from the environment and it all needs to be sampled.
How can the immune cells keep up with all this sampling when they are covered and surrounded by trillions of microbes in the gut?
The only way for the immune system to do its job effectively is to have the neighborhood watch, whereby the microbes in the gut communicate with the immune cells and direct them to the areas where sampling needs to occur.
The microbiota help to train and develop the immune system so that it understands what is normal in that environment and what is new and a potential problem.
This crosstalk indicates the intimate relationship between the gut micrbiota and the immune system.
Importantly, if there is dysbiosis in the microbiome, this will surely affect the functioning of the immune system.
How do these concepts apply to the severe respiratory disease that seems to be going along with Covid?
The virus enters the body by breathing in droplets from infected people. Anything we breath in will also end up in the gut to some extent, because when we breath in anything, it gets trapped by mucus.
Remember – everything inside the body is covered by a mucus layer – in which sampling occurs. In the lungs, there is an apparatus called the mucociliary elevator. The tiny cilia in the lungs are constantly waving and moving the mucus up and out of the lungs (in order to clean and move toxins along). They go into the sinuses and then get swallowed and drain out into the gut.
The bolus of mucus that we swallow from anything entering through the nose, ears and lungs gets sampled and classified as either friend or foe.
We know that 53% of the cases of Covid-19 present with gastro symptoms (like nausea, diarrhea and/or cramping) before any other symptoms – so it is clearly entering through the gut.
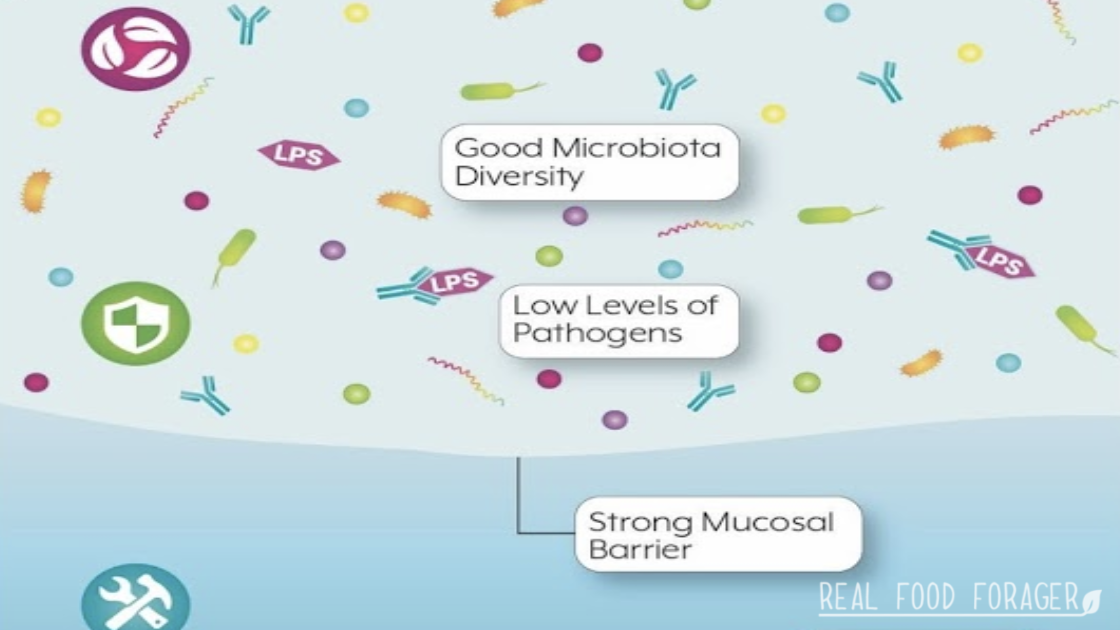
It follows that if the gut microbiome and gut mucosa are healthy, the immune system will function better and be able to address a pathogen like Covid-19 without a cytokine storm.
Of course we don’t know this yet, but we do know that the disruption of the gut microbiota (dysbiosis) is implicated in many chronic and inflammatory disease like obesity, diabetes and heart disease. (source)
We also know that the gut mucosa – the barrier – is essential in protecting against diseases and that leaky gut is a precursor to disease. (source)
We also know that lipopolysaccharide (LPS) can be used as a marker of leaky gut and inflammation and that many or us suffer from this foundational condition.
So it should come as no surprise that people who are seemingly “healthy” have succumbed to this new pathogen. It turns out that many people have chronic conditions that have developed from their leaky gut.
Chiropractors and now functional medicine providers have been talking about leaky gut for decades. Now we are finally seeing the science and maybe in another 17 years conventional medicine will recognize this as a root cause of many many diseases.
In order to address these problems you have to get to the root cause – which starts with dysbiosis – an imbalance in gut flora.
There are three important issues to address here:
1- Correct dysbiosis and improve and maintain bacterial diversity
2- Repair the mucosal barrier
3- Increase Treg (T regulatory) cells and overall immune function
It is critically important to correct the dysbiosis as the first step. The most efficient way to do this is to, of course, clean up the diet, but also to use a spore based probiotic that will help to recondition the gut – rather than try to reseed the gut.
Reseeding or repopulating with the lacto and bifido strains does not work that well, because they die on the way down to the lower intestines and colon. They do not survive the stomach acids, bile salts, pancreatic enzymes and the body heat.
Think about it – if you have to refrigerate your probiotic, what happens when it goes into the body at 98.6º?
Correct Dysbiosis and Improve and Maintain Bacterial Diversity
Diversity in the microbiome is best achieved by increasing the diversity of the diet. Hazda tribes eat up to 600 different types of foods annually. They eat complex carbs from seeds, roots and tubers (and also animal products).
In the west we generally consume 15-20 different foods (and lots of processed foods with additives that harm the microbiome).
Diversity in the microbiome ensures resilience against opportunistic infections.
Spore bacteria are also effective for increasing diversity, competitive exclusion and gut reconditioning. Certain species increase during fasting periods.
A new study published in the International Journal of Phamaceutics, showed that by combining the probiotic Megaspore with the prebiotic MegaPrebiotic, the benefits of increased short chain fatty acids and the bacteria that produce them were expanded 10 fold.
Intermittent fasting has also been shown to increase diversity of microbiome. Certain bacterial species increase with fasting (16 hour fast).
Repair the Gut Mucosal Barrier
The mucous barrier has 2 layers, the top part is where the microbiome lives and also contains metabolites, LPS and immune cells. It has a liquid consistency.
The bottom part of the barrier is called the mucin 2 layer and is a thick, ge-like substance. This protects against microbes that might be in the lumen of the intestine and protects the one cell epithelial gut lining. This critically important mucosal barrier is made with glycoproteins which are made of 4 specific amino acids. These specific amino acids can improve the production of mucous and help repair the barrier.
They are: l-threonine, l-serine, l-proline, and l-cysteine – these 4 are very important in the construction of the mucous layer. (source)
An increase in the short chain fatty acid butyrate will also help repair the mucosal barrier. Butyrate helps increase the production of mucin. Butyrate is produced by the gut bacteria and is critically important for gut repair.
Spore bacteria increase production of butyrate. (source)
Specific oliogosaccharides can support diversity and increase certain critically important keystone strains of good bacteria like Akkermansia muciniphilia and Fecalibactium prausnitzii. (Source)
Increase Treg cells and SIgA for Better Immune Function
Spore bacteria help to increase strains of bacteria that increase Treg cells.
Increase secretory IgA by lowering stress, because stress hormones inhibit SIgA production. Do this by the use of meditation, yoga, mindfulness, massage, etc. Massage increases oxytocin by as much as 30%. When oxytocin goes up, stress hormones go down.
Other ways to increase secretory IgA: moderate exercise, choline, vitamin C, zinc, serum bovine immunoglobbulins (IgGs), beta glucan, protein and omega-3 fatty acids.
Get more exposure to environmental microbes – especially for young children. The more exposure they get to microbes, the stronger the immune system.
You might be interested in this post. Vitamin D is Associated with Reduced Intestinal Permeability and Extended Remission in Autoimmunity
The root cause of many diseases are minor or major perturbations in the gut ecology. This can lead to a cascade of symptoms and ultimately, disease.
The best way to treat this is to balance the microbiome to allow the body to naturally heal.
You may be interested in my ebook Heal Your Microbiome Optimize Your Health.
If you are a healthcare provider and are interested in the practitioner brand of spore probiotics called Mega Sporebiotic, please contact me at Jill at microbiomelabs.com. Full disclosure – I am an account manager for this company, because I believe their product is completely superior to most probiotics on the market.
A source for a product with the four amino acids suggested above is called MegaMucosa from Microbiome Labs. Ask your health care provider to source this product for you.
Here is a source for a spore based probiotic that is available over the counter.
Information for this article was taken from several interviews given by Kiran Krishnan, Chief Science Officer of Microbiome Labs. This one in particular.
You might also like:
Interview with Kiran Krishnan about Gut Commensal Spore Bacteria Probiotics.
Image courtesy of Microbiomelabs.com.

Inspire Your Real Food Healing Journey with my FREE Grain-Free Meals e-Cookbook and Getting Started email series and newsletter! Unsubscribe anytime. Privacy Policy