We need to balance gut flora to address chronic constipation and gut motility.
SIBO (small intestine bacterial overgrowth) is now recognized by integrative and functional medicine practitioners as a very real condition.
SIBO is a condition when normal bacteria that live in the large intestine translocate up into the small intestine where they do not normally reside.
However, it gets more complicated. The constipation aspect of SIBO occurs because of damage to the Migrating Motor Complex (MMC).
We now know that a majority of SIBO cases have the initial trigger from an acute case of gastroenteritis.
Acute gastroenteritis is caused by bacteria that secret a toxin called cytolethal distending toxin (CDT). This toxin has 2 portions. One of the portions (B portion), looks very similar to our nerve systems in the small intestine. Through molecular mimicry or cross reactivity, the body will attack both the toxin and itself and cause damage to the small intestine.
This is an autoimmune situation that triggers a longer lasting autoimmunity.
The Migrating Motor Complex is made of nerve cells called the ICC nerve cells – (interstitial cells of Cajal). These cells produce an electrical wave that cleans the small intestine by sweeping it out.
When the cells of the MMC are damaged, they can no longer clean and we get an accumulation of bacteria (both normal and pathogenic) or an overgrowth of bacteria which is SIBO.
So acute gastroenteritis is an underlying cause of SIBO. There are other causes but it is the number one cause.
Dr. Mark Pimental’s The New IBS Solution, is great place to start to learn about the options for treatment.
You might also be interested in, Is Your IBS Really SIBO (Small Intestine Bacterial Overgrowth)?
In order to address these problems you have to get to the root cause – which starts with an imbalance in gut flora.
There are four important issues to address here:
1- Repair the mucosal barrier
2- Improve and maintain bacterial diversity
3- Improve gut motility
4- Increase Treg (T regulatory) cells and overall immune function
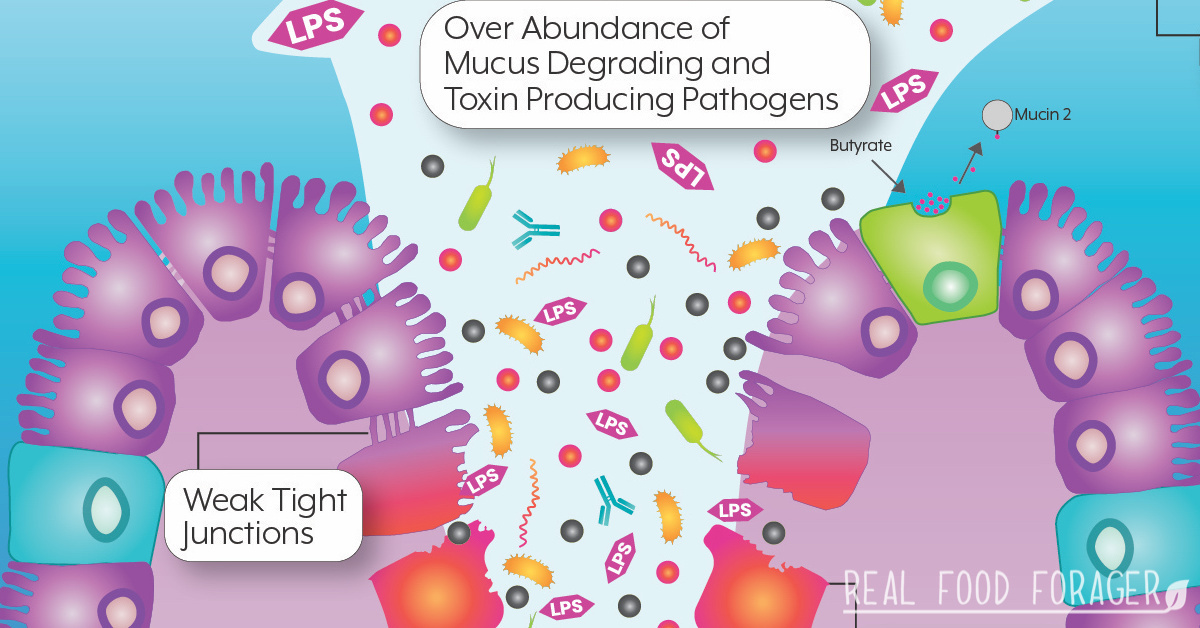
The mucous barrier has 2 layers, the top part is where the microbiome lives and also contains metabolites, LPS and immune cells. It has a liquid consistency.
The bottom part of the barrier is called the mucin 2 layer and is a thick, ge-like substance. This protects against microbes that might be in the lumen of the intestine and protects the one cell epithelial gut lining. This critically important mucosal barrier is made with glycoproteins which are made of 4 specific amino acids. These specific amino acids can improve the production of mucous and help repair the barrier.
They are: l-threonine, l-serine, l-proline, and l-cysteine – these 4 are very important in the construction of the mucous layer. (source)
An increase in the short chain fatty acid butyrate will also help repair the mucosal barrier. Butyrate helps increase the production of mucin. Butyrate is produced by the gut bacteria and is critically important for gut repair.
Bifidobacterium species can also utilize chondroitin sulfate and hyaluronic acid to make butyrate. So these two are considered prebiotics. People with SIBO who cannot tolerate resistant starches, may be able to take chondroitin sulfate and hyaluronic acid in order to increase butyrate.
Spore bacteria increase production of butyrate. (source)
Diversity in the microbiome is best achieved by increasing the diversity of the diet. Hazda tribes eat up to 600 different types of foods annually. They eat complex carbs from seeds, roots and tubers (and also animal products).
In the west we generally consume 15-20 different foods (and lots of processed foods with additives that harm the microbiome).
Diversity in the microbiome ensures resilience against opportunistic infections.
Spore bacteria are also effective for increasing diversity, competitive exclusion and gut reconditioning. Certain species increase during fasting periods.
A new study published in the International Journal of Phamaceutics, showed that by combining the probiotic Megaspore with the prebiotic MegaPrebiotic, the benefits of increased short chain fatty acids and the bacteria that produce them were expanded 10 fold.
Intermittent fasting has also been shown to increase diversity of microbiome. Certain bacterial species increase with fasting (16 hour fast).
There are several ways to improve gut motility:
Dietary changes – Increase in soluble dietary fibers from roots, green plantains, lima beans, brussel sprouts, asparagus, broccoli, carrots, apricots mangoes, prunes, etc.
Intermittent fasting (16 hour) – This helps gut motility because when you fast you are stimulating the MMC – the electrical wave that moves through the intestines and clears out the intestines.
Fasting in between meals – This is also important because when you eat a meal the MMC stops. So if you eat frequent small meals throughout the day, the MMC has stopped. Eating, then waiting 3-6 hours will suffice for the MMC to kick in again.
Prokinetics are important for increasing motility. These are; coffee, ginger root, garlic, magnesium and also exercise can have a stimulating affect on the bowels to get them moving.
Parasympathetic activation must be taken into consideration. People with fungal overgrowth and other opportunistic infections are sympatheic dominant. Parasympathics can be activated by humming, deep diaphragmatic breathing, cold water on face, gargling. Of course, addressing stress through meditation, yoga, and other means is also beneficial.
Spore bacteria help to increase Treg cells (source).
Increase secretory IgA by lowering stress, because stress hormones inhibit SIgA production. Do this by the use of meditation, yoga, mindfulness, massage, etc. Massage increases oxytocin by as much as 30%. When oxytocin goes up, stress hormones go down.
Other ways to increase secretory IgA: moderate exercise, choline, vitamin C, zinc, colostrum, beta glucan, protein and omega-3 fatty acids.
Get more exposure to environmental microbes – especially for young children. The more exposure they get to microbes, the stronger the immune system.
You might be interested in this post. Vitamin D is Associated with Reduced Intestinal Permeability and Extended Remission in Autoimmunity
The root cause of many diseases are minor or major pertubations in the gut ecology. This can lead to a cascade of symptoms including SIBO, chronic constipation and issues with gut motility.
The best way to treat these things is to balance the microbiome to allow the body to naturally heal.
You may be interested in my ebook Heal Your Microbiome Optimize Your Health.
If you are a healthcare provider and are interested in the practitioner brand of spore probiotics called Mega Sporebiotic, please contact me at Jill at microbiomelabs.com. Full disclosure – I am an account manager for this company, because I believe their product is completely superior to most probiotics on the market.
A source for a product with the four amino acids suggested above is called MegaMucosa from Microbiome Labs. Ask your health care provider to source this product for you.
Information for this article was taken from several interviews given by Kiran Krishnan, Chief Science Officer of Microbiome Labs.
You might also like:
Interview with Kiran Krishnan about Gut Commensal Spore Bacteria Probiotics.
Image courtesy of Microbiomelabs.com.

Inspire Your Real Food Healing Journey with my FREE Grain-Free Meals e-Cookbook and Getting Started email series and newsletter! Unsubscribe anytime. Privacy Policy